Disease: diabetic foot
Which organs are affected: blood vessels, joints, bones and nerves of the legs
Causes: diabetes, infection
Symptoms: dry, cracked skin on the legs, tingling, burning, pain, loss of sensation, gradual change in the shape of the legs
Complications: gangrene, amputation
Doctor: endocrinologist, orthopedist-traumatologist, vascular surgeon
Treatment: diet, physical therapy, drug treatment, surgical treatment
Prevention: timely check-up, proper foot care, hypoglycemic drugs, insulin therapy
Why does diabetes affect your feet?
Elevated blood glucose levels, characteristic of diabetes, can cause circulatory problems, affect nerve fibers and reduce their sensitivity. The result can be severe tissue damage. In this case, the feet turn out to be the most vulnerable, since they experience pressure from the weight of the whole body and are more often susceptible to injury (Fig. 1).
Figure 1. Development of diabetic foot syndrome. Source: CC0 Public Domain
In diabetes, a persistent, sometimes irreversible, decrease in sensitivity can develop. In such conditions, it is very easy to miss a pebble inside a sock or a blister on the foot. Because of this, cuts and ulcers may occur - the “entry” gate for any infection.
At the same time, insufficient blood flow to the legs and feet caused by diabetes aggravates the situation, making it difficult for wounds or ulcers to heal. An infection that gets into such a wound can quickly develop and lead to gangrene.
Diabetic foot: home treatment methods with orthopedic insoles
Treatment of diabetic foot with folk remedies is most effective when it is combined with wearing properly selected shoes. Often a person manages to significantly improve the condition of his limbs, get rid of ulcers and calluses, but uncomfortable or poor-quality shoes lead to the formation of new ulcerations in just a few hours.
Shoes should be made of high-quality material and not have thick seams. The size must be chosen exactly according to the foot.
Properly selected insoles are of great importance. For people with SDS, it is important to unload the feet and distribute the load evenly, as well as soften the shock waves that occur when walking and affect the arch and heel.
High-quality orthopedic insoles for diabetes will not only help to evenly distribute the load on the feet, but also promote their natural position in shoes, which avoids deformation of the joints, calluses and corns.
Regularly using unloading insoles in combination with traditional methods, you can achieve excellent results and prevent the development of the disease.
Click on the picture below to learn more about diabetic foot insoles and order them for home delivery or mail.
Benefits of using insoles for diabetic feet:
- reduction of pain when walking;
- preventing chafing of calluses;
- uniform distribution of the impact of body weight on the legs;
- preventing blood stagnation in the legs;
- correct position of the foot inside the shoe.
Who's at risk
The main reason for the development of diabetic foot is diabetes itself, which destroys nerves and affects blood vessels. An external factor in the appearance of SDS is infection (bacterial and fungal).
Important! Hypertension and atherosclerosis do not simply accompany diabetes, but are a consequence of metabolic disorders that develop with this disease.
Main risk factors:
- Duration of diabetes 10 years or more.
- Diabetic polyneuropathy is damage to peripheral nerves due to diabetes.
- Macro- and microngiopathy - pathology of vessels of large and small diameter cause, and stagnation of venous blood in varicose veins of the legs and lymphostasis further increase circulatory disorders. Hypertension with blood pressure more than 140/90 mm Hg. Art., like atherosclerosis, aggravate vascular damage in diabetes.
- Foot deformities of various origins, which provoke increased pressure on certain areas of the soles and toes. In areas of high pressure, calluses and thickening of the skin (hyperkeratosis) form, with the risk of subsequent injury and infection.
- Fungal infections, which are accompanied by cracks and thickening of the skin, contribute to ingrown nails with the subsequent development of purulent inflammation.
- Injuries, abrasions, burns due to decreased sensitivity and improper foot care.
- Impaired visual acuity in a patient, which makes it difficult to properly care for the skin of the feet and nails every day.
“The earliest and therefore most common complication of diabetes is diabetic neuropathy (nerve atrophy). It is this that often triggers a further cascade of pathological changes and serves as the basis for the development of such severe complications as diabetic foot,” warns Candidate of Medical Sciences, endocrinologist Larisa Aleksandrovna Marchenkova.
The development of SDS is also facilitated by:
- wearing uncomfortable, tight or too large shoes,
- smoking,
- alcohol consumption,
- heart and kidney diseases,
- obesity.
Contraindications to home treatment
Self-treatment at home is contraindicated for patients in whom the disease has developed to the first and higher stages. At initial symptoms or the appearance of minor lesions on the skin, the patient is advised to urgently visit the attending physician.
Treatment of the disease should be carried out under the supervision of a doctor, after an accurate diagnosis has been made. The patient, by following prevention methods, can avoid complications of the disease and prevent the disease from developing to the stage where it can only be treated surgically.
The article has been verified by the editors
What is diabetic foot like?
Depending on the main cause of the disease (damage to nerves or blood vessels), three forms of diabetic foot are distinguished (Table 1): neuropathic (predominant damage to nerves), ischemic (predominant damage to blood vessels) and mixed - neuroischemic (combined damage to blood vessels and nerves).
Table 1. Forms of diabetic foot syndrome
| Signs | VTS forms | ||
| Neuropathic | Ischemic | Neuroischemic | |
| Appearance of ulcers | |||
| Prevalence | 60-70% | 5-10% | 20-30% |
| Leather | Dry, warm, pink, calluses | Blue, cold | Pale, thin, cool |
| Deformations | Expressed specific | May exist, but are not specific | |
| Ripple | Saved | Absent | Reduced or absent |
| Location of ulcers | In areas of excess pressure | Upper surface of toes, heel area | |
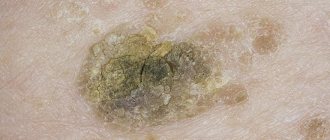
| Appearance of ulcers | Red, granulating, surrounded by necrosis | Covered with scab, total necrosis | Sluggish granulating, covered with necrosis and eschar |
| Pain in the area of the ulcers | No pain | Severe pain | Moderate pain |
Degree of damage
With DFS, the lesion begins in the skin, gradually spreading to the subcutaneous tissue, muscles, tendon apparatus of the foot, joints and bones.
Depending on the depth of the lesion, 6 degrees of ulcerative defects are distinguished (Table 2). Table 2. Degrees of development of diabetic foot syndrome
| Degree | Manifestations |
| 0 | There is no wound defect, but there is dry skin, beak-shaped deformation of the fingers, protrusion of the heads of the metatarsal bones, and other bone and joint changes |
| 1 | Superficial ulcerative defect without signs of infection |
| 2 | Deep ulcer (penetrates to the tendon or joint capsule), usually infected but without bone involvement |
| 3 | Deep ulcer with inflammation of bones (osteomyelitis) and joints (purulent arthritis) |
| 4 | Limited gangrene (within one toe or heel area), requiring minor amputation - at the level of the toes |
| 5 | Gangrene of the entire foot, when major amputation is necessary (above the ankle) |
There are other classifications that reflect not only the depth of the defect, but also the presence of infection and the degree of reduction in blood flow in the leg. These classifications are needed to determine the optimal treatment strategy for patients with DFS.
How to treat diabetic foot at home?
Recipes for getting rid of SDS are extremely varied. It is worth noting that before finding out how to cure diabetic foot at home, you need to remember what substances and products the body gave an allergic reaction to. It is strictly prohibited to use allergenic products for the treatment of SDS!
In most cases, traditional medicine (diabetic foot is an external disease affecting the epidermis of the extremities) advises the use of plant decoctions for washing wounds and baths.
Recipes for the most effective decoctions:
- Bird cherry berries 1 tbsp. spoon + 1 glass of water. Infusion time - 20 minutes.
- Rosemary 2 tbsp. spoons + chamomile leaves and flowers 2 tbsp. spoons + mustard flowers 2 tbsp. spoons + 1 glass of water. Leave for 10 hours.
- String + St. John's wort + plantain 2 tbsp. spoons + 1 tbsp. water. Leave for 1-1.5 hours.
- Eucalyptus leaves 1 tbsp. spoon + 1 glass of water. Infusion time - 5 minutes.
- Sage leaves + cloves 1 tbsp. spoons + 1 glass of water. Leave for 20-30 minutes.
- Gingo leaves 2 tbsp. spoons + cinnamon 0.5 teaspoons + 1 glass of water. Infusion time - 10 minutes.
- Currant leaf + young nettle + 1 liter of boiling water. Leave for 10-20 minutes.
- Swamp suschitsa 5 tbsp. spoon, pour 1 liter of water and leave for 10 minutes.
- Needles of any tree + 1 liter of boiling water. Leave for 30 minutes.
- Aloe juice 1 tbsp. spoon + 1 glass of warm water.
The prepared decoction is infused for the specified time, then filtered through a sieve, and used for baths or washing of ulcers, abrasions, scratches, and wet calluses. After washing, gently pat the skin dry with a soft towel.
Herbal decoctions are great help when the first signs of diabetic foot appear; when ulcers appear, it is more effective to use other folk remedies.
Symptoms: when to see a doctor
When you have diabetes, it is important to examine your feet every day and visit your doctor regularly to catch symptoms of diabetes.
You should make an appointment with your doctor immediately if you notice:
- Tingling, burning and pain in the legs,
- Pain or cramping in the buttocks, thighs or calves during physical activity,
- Loss of touch or the ability to feel heat or cold,
- Gradual change in the shape of the legs,
- Hair loss on toes, feet and legs,
- Dry, cracked skin on the legs,
- Change in color and temperature of your feet,
- Thickened yellow toenails
- Signs of a fungal infection, such as between the toes,
- A blister, wound, ulcer, infected callus, or ingrown toenail.
Most people with diabetes can prevent serious complications by starting treatment early.
There are also a number of signs that can be used to determine not only the presence of SDS, but also its form.
The neuropathic form usually develops with long-term diabetes and is accompanied by deformation of the feet and fingers. The sore foot is swollen, the skin is warm and dry to the touch, there are areas of hyperkeratosis and dry calluses. Ulcerative defects often form in places of excess pressure - areas of projection of the metatarsal bones, distal (terminal) phalanges of the fingers. Temperature and tactile sensitivity are reduced, pulsation in the arteries of the feet is preserved. The ulcers are painless, and thickening of the skin is often present around the defect. Leg pain in the neuropathic form occurs at night, accompanied by numbness, sensory disturbances, and cramps in the calf muscles.
The ischemic form of diabetic foot appears against the background of cardiovascular diseases - coronary heart disease, hypertension, atherosclerosis and obesity. The skin of the affected foot is cold, pale, with a bluish tint. Pulsation in the arteries of the feet is reduced or absent, sensitivity is preserved. Skin defects are most often localized in the terminal phalanges of the fingers, in the area of the heel, ankle, I and V metatarsophalangeal joints. The ulcers are often dry, covered with brown or black scab, and sharply painful. Leg pain in the ischemic form of DFS occurs during physical activity, and in advanced cases, at rest.
The neuroischemic form is mixed, combining the symptoms of neuropathic and ischemic forms of diabetic foot.
Very often, patients with diabetes, especially those with sub- or decompensated diabetes, experience serious skin problems. The question often arises: how is a carbohydrate metabolism disorder - diabetes mellitus - related to dry skin and skin infections to which they are susceptible? After all, all this indicates a violation of the barrier, protective function of the skin, or rather, the state of the epidermis and even its upper, horny layer. And why does the skin suffer when blood sugar levels are high?
Read the article
Which doctor should I go to?
Patients with diabetes are monitored by a primary care physician and an endocrinologist. It is necessary to examine the skin of your feet at every visit to the clinic. If signs of diabetic foot appear, do not wait for a routine examination: consult a doctor immediately! If an ischemic form is suspected, consultation with a vascular surgeon is necessary. In case of osteoarthropathic variant of the neuropathic form, you need to contact an orthopedic traumatologist. A neurologist, cardiologist and ophthalmologist should examine a diabetic patient at least once a year.
Diagnostics
To determine the clinical form of DFS and patient management tactics, the following are carried out:
- Careful history taking. The doctor clarifies the form and duration of diabetes mellitus, the severity of carbohydrate metabolism disorders, the nature of pain in the feet, the presence of ulcers in the past, changes in skin sensitivity, and the presence of visual impairment.
- Examination of both legs. Palpation is required to assess pulsation in the arteries of the feet and skin temperature.
- Detection of diabetic polyneuropathy includes assessment of the Achilles and knee reflexes and various types of sensitivity: pain, temperature, vibration, tactile.
- Instrumental assessment of the condition of the arteries of the legs includes ultrasound scanning of blood vessels and x-ray examination of the main arteries to determine the degree of narrowing.
- X-ray assessment of osteoarthropathy, the condition of the osteoarticular apparatus of the foot. Additionally, magnetic resonance imaging of the foot is used, and ultrasound densitometry (measuring bone density) is used to assess the degree of osteoporosis - decreased bone density.
- Bacteriological examination of the substrate discharged from the wound helps to determine the pathogen and its sensitivity to antibiotics.
Laboratory blood tests for sugar, glycated hemoglobin, and lipid profile are performed periodically to monitor the state of carbohydrate and fat metabolism.
Treatment
The success of treatment of diabetic foot syndrome depends on the joint efforts of the patient and continuity in the work of doctors - endocrinologist, cardiologist, neurologist, therapist. Important conditions for a good result are compensation of carbohydrate metabolism, patient compliance with diet, lifestyle recommendations, and cessation of smoking and alcohol. Sore feet should be carefully looked after, washed and trimmed on time. You should also consider changing your shoes if they cause discomfort. In some forms of the disease, wearing orthopedic shoes is indicated.
Diet
Diabetic foot syndrome occurs due to high blood sugar, so treatment involves following dietary recommendations. Confectionery products, sweets, white bread, pasta, animal fats, smoked foods, mayonnaise, spicy, fried and salty foods are contraindicated. It is possible to use sugar substitutes, but not fructose, xylitol and sorbitol (they are very high in calories, and fructose increases blood sugar levels).
Important! Patients with diabetic foot benefit from lean meats and fish, vegetables (limiting potatoes), low-fat dairy products, some cereals (buckwheat, pearl barley, oatmeal), berries and fruits (except sweet ones - watermelons, grapes, bananas).
Therapeutic exercise (physical therapy)
Sport improves microcirculation in the vessels of the feet, strengthens weakened muscles and joint ligaments, stimulates lymphatic drainage and prevents the progression of pathological processes in the foot. In addition, physical exercise can reduce elevated sugar levels and improve cell sensitivity to insulin. It is important not to overdo it with exercise, take into account the degree of increase in blood pressure, pulse, and sugar levels. If the pressure is above 140/90, the pulse is more than 80 beats per minute and the blood sugar is above 15 mmol/l, it is not advisable to start a course of therapeutic exercises.
You should not inject insulin before exercising. It reduces glucose levels, and muscles need it as a source of energy. You need to exercise every day for at least 15–20 minutes. The complex is selected individually, taking into account the severity of diabetes and complications. Swimming and moderate walking are beneficial.
Drug treatment
Drug treatment should primarily be aimed at compensating for carbohydrate metabolism disorders. Additionally, correction of blood pressure, lipid metabolism disorders, the use of antibacterial drugs in case of infection development, means to improve blood microcirculation, anti-inflammatory and analgesic drugs will be required. For ulcers, they resort to local remedies.
Among the medications prescribed for the treatment of SDS:
- Insulin and hypoglycemic drugs. With the development of diabetes mellitus in patients with type 2 diabetes mellitus, timely transfer from glucose-lowering drugs, which at some point stop helping, to insulin therapy is important.
- Antihypertensive drugs are used to maintain blood pressure within the upper limit of normal - no more than 140/85 mmHg. It is better if these medications are prescribed by a cardiologist after an ECG.
- Lipid-lowering drugs (statins, omega-3, nicotinic acid, etc.) are needed to correct lipid metabolism disorders with increased levels of cholesterol, triglycerides, and low-density lipoproteins.
- To prevent thrombosis and improve blood circulation in small vessels, heparin, acetylsalicylic acid, prostaglandin E1, etc. are used.
- Antibacterial therapy is carried out taking into account the sensitivity of pathogens inhabiting the wound to antibiotics. To suppress them, drugs of protected penicillin, cephalosporins of 2–4 generations, fluoroquinolones, sulfonamide drugs, and carbapenems are used.
- To relieve pain, nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics (including narcotics), and anticonvulsants (some of them have an analgesic effect) are used.
Local treatment using special dressings plays an important role in the treatment of defects in DFS. This excludes the use of gauze, alcohol-containing products, and ointments. When choosing a dressing, they are guided by the principle of wet healing of ulcerative defects. Calcium-alginate dressings are used to remove excess fluid from the wound; hydrocellular dressings are used to treat superficial wounds. For ulcers with necrotic scab and dense fibrinous plaque, hydrocolloid dressings help. The preferred antiseptics are ionized silver and povidone-iodine.
Surgery
Surgical treatment options for DFS depend on the form and stage of the disease. The following operations are used:
- Opening abscesses and phlegmons - purulent lesions of the skin, subcutaneous tissue, and periarticular tissues of the foot.
- Necrectomy – removal of limited areas of necrosis (death) of foot tissue.
- Skin grafting operations to close wounds or ulcers on the foot.
- Surgeries on the blood vessels of the legs to restore the deficiency of arterial blood flow.
The latter include:
- Balloon angioplasty and stenting are interventions that are performed on blood vessels under X-ray control. Under local anesthesia, a puncture is made, a conductor is inserted into the artery, through which the lumen of the vessel is restored using a balloon or stent (tube).
- Bypass surgery is the restoration of blood flow in the femoral and popliteal arteries by replacing part of the affected vessel with a prosthetic tube. Such operations are performed under general anesthesia using a heart-lung machine.
The main indications for angiosurgical interventions are a critical level of blood flow in patients with neuroischemic or ischemic forms of diabetic foot.
Folk remedies, hirudotherapy
Using only folk remedies (herbal medicine) for SDS is pointless. As an addition to the comprehensive treatment of type 2 diabetes, green bean pods, blueberries, oats, flaxseed, bay leaves, burdock, and clover can be used in the form of infusions and decoctions for oral administration. Freshly squeezed juices are useful (tomato, cucumber, carrot with the addition of Jerusalem artichoke, parsley, celery, lettuce, Brussels sprouts, green beans).
When using hirudotherapy (leech treatment), cleansing and healing of the ulcer occurs 2 times faster. This is explained by the entry into the blood of many enzymes with antithrombotic, antisclerotic, vasodilating, analgesic, anti-inflammatory and anti-edematous effects.
Treatment with honey
Foot baths with honey are considered an effective remedy. For every liter of warm water add 2 tbsp. fake product. A decoction of dry eucalyptus leaves can be added to the resulting solution.
You should not add salt to such baths, as the crystals can scratch the skin.
The product is also used to eliminate swelling of the lower extremities. To do this, the “sick” leg is lubricated with linden honey. A layer of pre-crushed Acetylsalicylic acid tablets is applied on top. Everything is fixed with burdock leaves and wrapped with a gauze bandage. The manipulation is carried out twice a day, and after swelling decreases - 1 time.
Another effective remedy is a combination of honey, xeroform and fish oil. The weight of the ingredients is 80 g, 3 g and 20 g, respectively. Mix to obtain a homogeneous consistency. The resulting product is applied to gauze or a natural piece of fabric and applied to the defects.
Honey is a product that is a storehouse of nutrients for healthy and sick people.
Prevention
It is better to start fighting diabetic foot even before it appears. To do this, you need to remember a few simple things.
Important! Any patient with diabetes or impaired glucose tolerance (determined by an appropriate test) should carefully monitor the skin of the legs, because even minor inflammation can lead to amputation.
Daily foot examination
Check your feet daily for cuts, redness, swelling, sores, blisters, corns, calluses or any other changes to the skin or nails. If you can't see your feet clearly, use a mirror or ask someone to help.
“The loss of sensation in a patient with diabetic foot can be so severe that he cannot feel the terrain under his feet. Paving stones, asphalt, sand - he feels it all like cotton wool. The shoes press, the folds of the sock rub, but the person doesn’t feel any of this. He can put his foot on a hot radiator and fall asleep, and wake up with a fourth-degree burn, in which the tissues of the foot are burned to the bone, but there is no pain! This is why I recommend that diabetic patients examine their feet daily using a foot mirror. This should become the same habit as brushing your teeth,” advises Doctor of Medical Sciences, Professor, Head of the Endocrinology Department of the State Budgetary Institution “City Clinical Hospital named after A.K. Eramishantsev of the Moscow Department of Health” Leonid Yulievich Morgunov.
Hygiene
Take proper care of your feet. Wash your feet daily with soap, dry them gently and dry the spaces between your toes, and change your socks. This will help avoid infection in emerging wounds.
To treat wounds, do not use iodine, brilliant green and alcohol, as they tan the skin. Microtraumas can be treated with solutions of hydrogen peroxide, chlorhexidine, dioxidine, miramistin.
To soften calluses, do not use acidic or alkaline products, and do not cut them with a razor.
Dry skin of the feet should be lubricated with nourishing creams, as well as products with urea.
Pedicure
Caring for the skin of the feet and nails for diabetes is not only an aesthetic, but also a therapeutic procedure. It is carried out by a special specialist – a podiatrist (Fig. 2). It removes corns and dry calluses, which helps reduce stress on the soles and prevent cracks. At the same time, regularity of pedicure is important - once every 2-3 weeks.
Basic rules for pedicure for diabetes:
- The temperature of the water for the bath is 36–37 C0, the duration of its use is 6–7 minutes. You can add antiseptic and softening oils to the water.
- Do not use a razor to remove keratinized skin. You can use fine-grained pumice or a sanding file, or use disposable fine-grained attachments for hardware pedicure.
- Trim your nails roundly, not straight (if you leave corners, they will grow into the skin of your fingers, causing inflammation), file the free edge of the nails from the corner to the center.
- Use antiseptics without alcohol.
Figure 2. Pedicure from a specialist. Source: CC0 Public Domain
Shoe selection
To prevent damage to the skin, it is important to use comfortable shoes: do not buy tight or narrow shoes, with thin and soft soles. It should be soft, made from natural materials, and match the size of the foot. It is better to choose shoes in the afternoon, when the foot swells. If sensitivity is reduced, you can use a cardboard insole that follows the shape of the foot. Is the insole inserted inside deformed? Shoes can cause scuffs!
In case of foot deformation, transverse or longitudinal flatfoot, it is advisable to use orthopedic shoes or special insoles, except magnetic ones. It is important to inspect it inside every day to avoid compactions, folds, or deformations.
For neuropathic ulcers of the forefoot, unloading is required using individual orthopedic shoes of the “half shoe” type. Its design allows you to move on the affected limb. In this case, the load from the front of the foot is transferred to the heel area.
Important! Diabetic patients should not walk barefoot! This can cause serious damage to your feet.
Protection of feet from cold and heat
If you have developed nerve damage as a result of diabetes, you may burn your feet without even realizing it. To protect your feet from burns:
- Wear shoes on the beach and on hot asphalt,
- Apply sunscreen to your feet to prevent sunburn.
- Keep your feet away from heaters and open flames,
- Don't put a heating pad on your feet.
Cold weather can also cause damage to your feet. Wear socks to bed if your feet are cold. In winter, wear waterproof, lined boots to keep your feet warm and dry.
Free blood flow to the legs
Follow these tips to improve blood flow to your legs:
- When you are sitting, raise your legs up (use a pouf)
- Wiggle your toes for a few minutes throughout the day. Move your ankles up and down, in and out to improve blood flow in your feet and legs,
- Do not wear tight socks or elastic stockings,
- Play sports. Choose activities that you enjoy, such as walking, dancing, yoga or stretching, swimming or cycling,
- Do not smoke.
Sources
- Bulletin of the International Scientific Surgical Association Vol.3, N. 2-3, 2008 The Fifth International Scientific Distant Congress on Spine and Spinal Cord Surgery “InterSpine - 2008”, The Sixth International Scientific Teleconference “Cardiovascular Surgery and Angiology - 2008” Saint -Petersburg, Russia, December, 2008 - 33 - © Kislyakov VA, 2008.
- Marchenkova L.A. et al. Improving integrated approaches to the treatment and medical rehabilitation of patients with diabetic neuropathy. Journal “Attending Physician” No. 12–2017, https://www.lvrach.ru/2017/12/15436869
- Dedov I.I., Udovichenko O.V., Galstyan G.R. Diabetic foot. M.; 2005.
- International agreement on diabetic foot. Compiled by the International Diabetic Foot Working Group. M.; 2000.
- BULLETIN OF NEW MEDICAL TECHNOLOGIES – 2007 – T. XIV, No. 3 – P. 152