Causes
According to ICD-10, the reason that periarthritis of the shoulder joint occurs is prolonged overstrain of the muscles in the area of the shoulder joint, as well as increased movements of the arms. These factors create microtraumas of tendon fibers, internal hemorrhages and others create conditions for swelling of periarticular tissues and circulatory disorders, which leads to the development of periarthritis.
Also the cause is prolonged trauma in the area of the ligamentous-tendon area of the described joint. Another reason is the degenerative processes of tendon fibers in the cervical spine caused by cervical spondylosis, osteochondrosis and diseases of individual organs - for example, the problem can develop as a consequence of a heart attack, angina pectoris, and so on.
But ICD-10 does not identify the problem as a separate nosology, since there can be many causes of dysfunction of the shoulder joint. ICD-10 classifies the following pathologies and abnormalities as periarticular lesions in this area:
- calcific type tendinitis;
- adhesive capsulitis;
- impingement syndrome;
- bursitis of the shoulder joint and a number of others.
Treatment of periarthritis of the shoulder joint at home with folk remedies
Shoulder periarthritis is an inflammatory pathology that, if left untreated, takes on a degenerative-dystrophic nature. A person suffers from pain that intensifies with movement, making it difficult to sleep peacefully at night. Periarthritis responds well to conservative treatment with drugs of various clinical and pharmacological groups. The patient is prescribed anti-inflammatory nonsteroidal drugs (NSAIDs), muscle relaxants, and chondroprotectors. To eliminate severe pain and relieve an acute inflammatory process, glucocorticosteroids are injected into the tendon or cavity of the shoulder joint.
The drugs have a wide range of contraindications, and systemic and local side effects occur. Therefore, at the remission stage, shoulder periarthritis is treated with folk remedies. Infusions of medicinal herbs, compresses, rubs, and homemade ointments are used.
Symptoms of mild (simple) form
The described glenohumeral periarthritis has different degrees of severity. The mildest is considered to be the so-called simple (mild) glenohumeral periarthritis, the form that is easiest to correct and proceeds favorably. The main symptoms of the simple form are:
- minor pain in the shoulder area (they cannot be felt unless you move your hand);
- increased pain when even slightly raising the arm or when rotating in an extended form;
- a feeling that movement in the joint is limited, in particular, it is impossible to place the hand behind the back far enough.
A person may not pay attention to such symptoms, considering them insignificant. This can lead to negative consequences - glenohumeral periarthritis will develop into an acute form. According to statistics, this happens in 60% of cases, so it’s worth paying attention to even subtle symptoms that the body sends.
Humeroscapular periarthritis
Other treatments
If the cause of pain is muscle rupture, then conservative treatment is ineffective. In this case, surgical intervention with stitching of muscle fibers is provided. Today, the most commonly used low-traumatic technique is arthroscopy. The device is inserted into the joint area through small incisions in the skin.
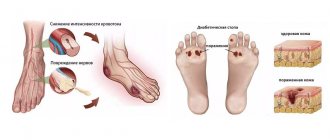
According to clinical statistics, periarthritis of the ankle, hip or knee is much less common compared to inflammation of the periarticular soft tissues of the shoulder. It is worth noting that doctors also often associate constant pain in the joints of the lower extremities with arthritis or arthrosis.
Clinically, periarthritis of the foot, knee or hip joints will usually manifest itself as pain, dysfunction and, in the later stages, muscle atrophy, so the approach to treatment will be identical to that for inflammation of the periarticular tissues of the shoulder.
If you do not know how to properly treat periarthritis of the shoulder, elbow, hip or ankle joint, then consult an orthopedic doctor to avoid worsening the condition.
Acute symptoms
As mentioned earlier, the acute form of the disease occurs after the deterioration of the simple form. It is usually caused by injury or excess stress. But sometimes it arises on its own. Its most characteristic signs are usually:
- almost complete impossibility of rotating the hand with the remaining ability to painlessly move it forward;
- increasing pain step by step, occurring suddenly and spreading mainly along the arm and neck;
- increased pain at night;
- a small swelling located on the front side of the shoulder;
- general deterioration of the condition, especially the development of insomnia;
- a small but noticeable increase in temperature (does not always occur).
The development of the acute form lasts several weeks. Mobility can be partially restored if the person is treated and given therapeutic exercises. Humeral periarthritis may continue to develop, then it will worsen and turn into its chronic form.
Symptoms of the disease and stages of formation
The first stage is called “simple painful shoulder.” This is the initial stage of shoulder joint disease.
The process begins with inflammation of the tendons of the infraspinatus and supraspinatus muscles of the shoulder joint. In some cases, tendonitis of the head of the biceps muscle appears.
The main symptom is pain in the shoulder joint, which intensifies with active movements of the arm. Often, radiographic examination does not reveal pathological abnormalities at this stage.
If glenohumeral periarthritis is detected at the initial stage, then treatment takes a short period - up to 7 days. If treatment is started later, there is a risk of the disease becoming acute or chronic.
The second stage of the disease is called “acute painful shoulder.” The condition can occur independently or be a consequence of untreated primary glenohumeral periarthritis.
At the acute stage, the bursa and tendons of the shoulder joint become inflamed, and the affected tissues begin to calcify. Often the pain is unexpected. Pain appears after strenuous physical activity on the joint.
After some time, the pain intensifies in the back of the neck and arms. At night, the pain can increase, causing great discomfort.
The acute stage of glenohumeral periarthritis is characterized by the fact that the motor activity of the arm is significantly reduced, except in the forward direction.
In the acute stage of the disease, baths or compresses from the arsenal of traditional medicine are quite effective. As is known, these methods must be used carefully, combining them with drug therapy.
Periarthritis is divided into several forms and stages of development.
- The so-called “simple painful shoulder” implies the initial stage of a disease of the shoulder joint, which develops most often in patients. During the process itself, inflammation of the tendons of the supraspinatus and infraspinatus muscles of the shoulder joint occurs; less commonly, tendonitis of the head of the biceps muscle may occur. A symptom of the disease at this stage of its development is pain in the shoulder joint, and its intensification with active movement of the arm, while an x-ray examination may not reveal any pathological abnormalities. If glenohumeral periarthritis is detected at the initial stage, its treatment can take a fairly short time, up to 1 week. If the disease is not treated in a timely manner, it may transform into a chronic or acute form.
- “Acute painful shoulder” - occurs both independently and is a consequence of untreated initial glenohumeral periarthritis. During the acute stage, inflammation of the bursa and tendons of the shoulder joint occurs, as a result of which the affected tissues become calcified; pain often manifests itself unexpectedly, mainly this occurs after heavy physical exertion on the affected joint. The pain increases over time in the area of the back of the arm and neck. At night, the pain may intensify, causing quite a bit of discomfort. During the acute stage of glenohumeral periarthritis, hand movements are almost completely limited, except in the forward direction. In this case, some compresses or baths from home folk remedies can help, but these measures should be taken carefully, and consult a doctor for qualified treatment as soon as possible. You can also relieve pain by placing your arm in a physiological position, bending it and applying it to your body.
Symptoms of the chronic (permanent) form
When chronic glenohumeral periarthritis begins to manifest itself, its symptoms are as follows:
- the pain in the arm becomes moderate, not causing unnecessary discomfort;
- at night it begins to ache in the shoulder area, this may prevent the patient from sleeping;
- With inaccurate rotations and simple hand movements, the sore shoulder begins to give off particularly acute pain.
Humeral periarthritis lasts from several months in an optimistic case to several years in a pessimistic case, until it goes away. But if the problem is not treated, then capsulitis may occur, popularly called “frozen shoulder” - this happens in 30% of cases. “Frozen shoulder” is the final, most severe stage that scapulohumeral periarthritis can have, in which the limb becomes immobilized, so timely treatment of periarthritis is mandatory.
Causes of the disease
The appearance of glenohumeral periarthritis is provoked by the following factors:
- Age over 40 years (especially in women),
- Hypothermia of the joint,
- Staying in a damp room for a long time,
- Malformations of the upper shoulder girdle,
- Mental illnesses,
- Nervous system disorders
- Arthrosis,
- Spondylosis,
- Sciatica.
Humeroscapular periarthritis often appears in athletes who receive macro- and microtraumas during their active professional activities.
Diagnostics
If the symptoms described above make themselves felt and there is a serious suspicion of periarthritis of the shoulder joint, in this case the patient can choose to consult one of the doctors: a surgeon, therapist, as well as a rheumatologist, traumatologist, orthopedic specialist or neurologist.
To begin with, the specialist will collect an anamnesis, perform palpation, assess the activity of the shoulder joint and evaluate it visually. If clarification is necessary, radiography, MRI or ultrasound can be performed. An x-ray can show changes characteristic of a developed chronic form - the doctor will identify deposits of calcium microcrystals (the so-called calculous bursitis). If periarthritis of the shoulder joint is present in acute form, the composition of the blood changes.
Shoulder arthroscopy
Invasive (penetration) diagnostic methods are also possible, for example, arthrography or arthroscopy. They are done to exclude arthrosis, arthritis, arterial thrombosis, and Pancoast syndrome, which have similar symptoms.
No. 7: nettle infusion
If you have nettle growing on your property, then when weeding, do not rush to throw it into the compost heap. Instead, dry the leaves of this actually very healthy plant and use it to make a nettle infusion for periarthritis.
Read also: Arthritis of the ankle
Take 20 grams of crushed dry nettle herb per half liter of boiling water, mix thoroughly and leave to infuse for fifteen minutes. After this, the medicine is ready: strain it and take one tablespoon every eight hours.
In a similar way, you can use not only nettle, but also black currant leaves. To do this, take five grams of dry blackcurrant leaves and brew them in one glass of boiling water. Then, after stirring, leave the product to infuse for twenty minutes, and then strain, divide into two equal parts and drink them throughout the day.
Cure arthrosis without drugs? It's possible!
Get the free book “Step-by-step plan for restoring mobility of the knee and hip joints with arthrosis” and start recovering without expensive treatment and surgery!
Treatment
Periarthritis of the shoulder joint can be treated with folk remedies, or you can (and in some cases need to) turn to specialists. Then, when pathological glenohumeral periarthritis manifests itself, high-quality inpatient treatment will be provided.
Any therapeutic measures are aimed primarily at eliminating and preventing muscle contractures and relieving pain. With any approach, it is imperative to observe a gentle motor regimen, and in the acute stage, the arm is unloaded using a plaster splint or a special bandage.
Special bandage for unloading the arm
Self-treatment
Treatment with folk remedies, mainly at home, is carried out only in simple and chronic forms. The simplest and most popular methods of surgical treatment with folk remedies:
- rubbing the sore spot with calendula tincture, filled with vodka in a ratio of 1/10;
- compress on the sore spot from crushed horseradish root;
- infusion of crushed St. John's wort, poured with boiling water, taken orally;
- nettle infusion, heated in a water bath and taken orally.
It is important to remember that you should not replace physiotherapy with folk remedies at home, but supplement it.
The so-called post-isometric relaxation is also often used. Postisometric relaxation is a whole system based on muscle relaxation using a special technique. But to alleviate glenohumeral periarthritis, you can use a simpler set of exercises, for example:
- In a sitting position, place your palms on your waist, spread your elbows, move your elbows back and forth 5-6 times.
- Then make circular movements with your shoulders.
- Place the hand of the sore hand on the “healthy” shoulder, and with the healthy hand firmly grasp the elbow and pull it up.
A set of exercises for glenohumeral periarthritis
This is just one example of possible therapeutic exercises. Before performing exercises, it is better to consult a doctor so that glenohumeral periarthritis does not worsen.
Traditional treatment
General treatment, when periarthritis is detected, and not necessarily glenohumeral, is often carried out using injections of non-steroidal anti-inflammatory drugs. Corticosteroids and dimexide applications are also used.
Other different types of drugs may be prescribed, for example, muscle relaxants and angioprotectors, metabolic agents and chondroprotectors. Next, individually selected exercise therapy is prescribed for glenohumeral periarthritis, physiotherapy, including, for example, electrophoresis, magnetic therapy, laser therapy and other forms. Massage and sulfide/radon baths are prescribed. Shock wave therapy is gaining popularity. In some cases, surgical treatment may be prescribed to eliminate periarthritis of the shoulder joint.
Folk remedies in the fight against illness
Gelatin is essentially a natural component for building joints. It is effective for lesions of cartilage tissue. The patient's diet can include products with gelatin, for example, fruit jellies or jellied meats. Gelatin is also included in some tincture or compress recipes, so treating joints with gelatin makes sense.
Fasting is strictly prohibited. During illness, the body needs nutrients. Patients with glenohumeral periarthritis do not have their own diet, but it is known that they need to eat food rich in minerals, vitamins and calcium.
With proper treatment at home, combining it with the main therapy, you can quickly eliminate glenohumeral polyarthritis.
For example, to treat the shoulder joint, the method of hirudotherapy is used, this is treatment with leeches. This method allows you to improve microcirculation in tissues, accelerating the recovery process.
Some of the above remedies are used both topically and orally.
Warm compress with chamomile. For periarthritis, you need to grind 1 part marshmallow, 2 parts sweet clover and chamomile, then pour boiling water until a pasty state is obtained.
The resulting mixture is transferred to gauze or cloth and applied to the sore joint. To retain heat, cover the compress with film and a warm cloth. Keep the compress on the area until it cools completely.
Treatment with folk remedies involves the use of salt dressings, these are a kind of salt compresses on the joints. To do this you will need a soft cloth, water and salt. You need to add 100 g of salt to a liter of water, stir well, heat the solution to 38-40C, and soak a thick cloth or gauze in this liquid for several hours.
The bandage is applied to the painful joint and should be secured with a dry cotton scarf.
Baths with hay dust. 500-700 g of dust is poured into 10 liters of water and brought to a boil. After this, the broth is removed from the heat and infused for at least 1 hour.
The pre-strained liquid is poured into a heated bath, which should be taken for no more than 20 minutes. In this case, the water should not be too hot; the permissible water temperature is 37-38C.
Treatment with honey compresses is a fairly common method of treating glenohumeral periarthritis. The affected area and adjacent tissues should be coated with a thin layer of natural honey, wrapped in a plastic bag, and the joint well insulated with woolen cloth.
It is best to perform the procedure in the evening, shortly before bed. The compress is removed the next morning.
Compress of chamomile and sweet clover. 2 tablespoons of chamomile and 2 tablespoons of sweet clover are poured with boiling water and infused for at least 1 hour.
This recipe does not require a decoction, but the pulp that results from it. This paste is applied to the affected area as a compress and removed after 2 hours.
Burdock leaf compress. Burdock should be as fresh as possible. The sheet is washed well and heated, after which it is applied to the affected area and a compress is fixed. Burdock leaf can be kept on the body all night and removed in the morning.
The occurrence of glenohumeral periarthritis can be caused by several factors:
- For the most part, patients with this disease are women over 40 years of age.
- Hypothermia of the joint.
- Prolonged stay in an environment where there is increased dampness.
- The presence of certain diseases, such as: congenital malformations of the upper shoulder girdle, which includes the shoulder joint.
- Neuropsychiatric diseases.
- Sciatica.
- Arthrosis.
- Spondylosis.
Humeral periarthritis is also quite often suffered by people in sports professions who receive micro and macro injuries that manifest themselves in the course of their professional activities. However, glenohumeral periarthritis can occur without any apparent reason, then it is very important to detect the disease in time and begin its treatment.
With proper treatment with home remedies coupled with pharmaceutical ones, you can quickly cope with glenohumeral periarthritis. For example, when treating the shoulder joint, the method of hirudotherapy, that is, treatment with leeches, is quite common, in this way you can improve microcirculation in the tissues and speed up the healing process.
- Warm herbal compress with chamomile. For periarthritis, treatment with a compress according to the following recipe helps: crushed herbs in the proportion of 1 part marshmallow, two parts each of sweet clover and chamomile, pour boiling water until a mushy mass forms. After this, transfer the resulting mixture to a clean piece of gauze or cloth and apply it to the sore joint; to preserve heat, cover the compress with film and a warm cloth. After the compress has cooled completely, remove it from the body.
- Treatment with folk remedies using salt dressings. For this you will need salt, water and a soft cloth. Add 100 g of salt to 1 liter of water, stir until completely dissolved, and soak in the solution several layers of gauze or thick fabric, preferably linen, for several hours. Heat the solution to 38-40C, remove the warm bandage from the liquid and apply it to the sore joint, securing it with a dry cotton scarf.
- Traditional treatment with hay dust baths. Pour 500-700 g of hay dust with 10 liters of water and bring to a boil, then remove the container from the heat and steep the broth for 40-50 minutes. Pour the strained infusion into a pre-filled bath, which should be taken for no more than 20 minutes, and the water should not be hot, within 37-38C.
- Home treatment with honey compresses. For glenohumeral periarthritis, you can coat the painful area and nearby tissues with a thin layer of natural flower honey, then cover everything with a plastic bag, and insulate the joint with a woolen scarf on top. It is advisable to perform the procedure in the evening before going to bed; remove the compress in the morning.
- herbal decoctions,
- baths,
- compresses.
We invite you to familiarize yourself with: Comminuted fracture Definition Types Causes Diagnosis Treatment Prognosis
Warm compress with chamomile. For periarthritis, you need to grind 1 part marshmallow, 2 parts sweet clover and chamomile, then pour boiling water until a pasty state is obtained.